Click on the below link to self refer yourself for support with your alcohol use, this service is provided through BDP.
HIV testing – why am I being asked?
You may find yourself being asked at your next blood test appointment if you would like a HIV test as part of the bloods you are having. In case you are wondering why, this is part of a nationwide campaign to raise awareness for everyone of their own HIV status, it is not designed to target one specific group of patients, everyone is being invited to have one.
For more information on HIV awareness and testing please view the links below:
https://www.england.nhs.uk/blog/a-routine-blood-test-not-only-changed-annes-life-but-saved-it
https://www.nhs.uk/conditions/hiv-and-aids
If you are of African or Caribbean heritage, you can also take advantage of free STI screening with ‘Common Ambition’, at MHC, on the first Thursday of each month.
Details below:
Cervical Screening
Cervical screening tests for human papillomavirus (HPV).
HPV is very common. Most people will get the virus at some point in their life. It is spread through close skin to skin contact during any type of sexual contact. There are many different types of HPV, some types can cause abnormal cell changes, but only some types can lead to cancer, these types do not cause any symptoms. In most cases, your immune system can get rid of the virus without you ever knowing you had it.
Sometimes HPV can stay in the body for many years at undetectable levels without causing any problems. This is called ‘dormant’ HPV. Dormant HPV can become active and is then found at screening. This means the HPV infection can become active again years after you have it. HPV can cause abnormal cell changes in your cervix.
Your cervix is the lowest part of your uterus (or womb), and it is found at the top of your vagina.
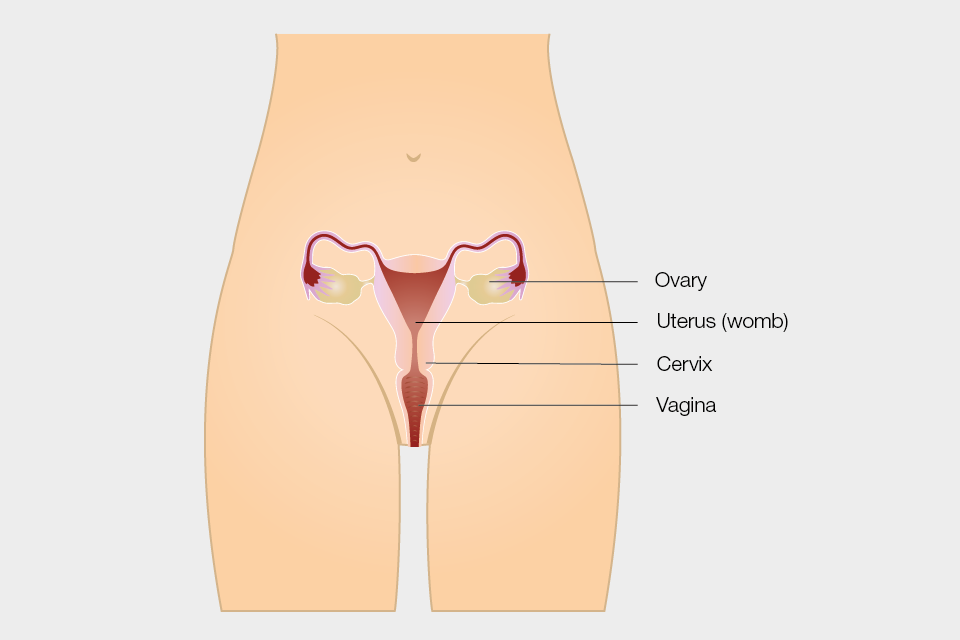
Diagram showing the female reproductive system.
Your body can usually get rid of the abnormal cells and your cervix returns to normal. But sometimes this doesn’t happen, and the abnormal cells can go on to develop into cancer. This is usually a slow process taking over 10 years.
Going for cervical screening when invited is the best way to protect yourself against cervical cancer. It is your choice whether to have a cervical screening test or not. Please read the leaflet about cervical screening available at: Cervical screening: leaflet for women considering screening – GOV.UK (www.gov.uk). This leaflet will help you decide whether to have the test and provide more information about HPV and cervical cancer.
You will get an invitation for cervical screening through the post if:
- your contact details are up to date
- you are between 25 and 64 years old
- you are registered as female on your NHS records*
In some areas, you may be able to arrange your appointment at a sexual health clinic instead of your GP practice.
If you are not registered at a GP practice and would like to have screening at a GP practice, you will need to register first; more information about registering is available at: How to register with a GP surgery – NHS (www.nhs.uk)
In some areas, local sexual health clinics may also offer screening. More information about finding a sexual health clinic local to you is available at: Find a sexual health clinic – NHS (www.nhs.uk).
If you are not sure if you are due for cervical screening, you can ask your GP or health professional.
*If you have a cervix but are not registered as female with your GP you will need to ask for a cervical screening appointment. You can talk about this with your GP, practice nurse, at a sexual health clinic or transgender health clinic. More information is available at: NHS population screening: information for trans and non-binary people
Booking your appointment
Before you book your appointment, it might help to think about what would make screening easier for you. You might already know what can help or you may want to discuss this with a nurse or health professional who can make some suggestions. Here are some tips that might help:
- If you get anxious sitting in waiting rooms, let the receptionist know. You can ask to book the first appointment of the day, so that you do not have to wait long.
- If you would prefer to be seen by a woman, ask for a female health professional.
- Tell the receptionist if you would like a chaperone. This is a usually another health professional. You might also want a friend, relative or carer present.
- You may feel you need more time for your cervical screening appointment. Ask the receptionist if you can book a longer appointment to give you more time during and after.
You may also wish to consider asking for an appointment just to talk about what happens during the screening first (you do not have to have the test at this appointment).
If you find screening painful a doctor may be able to prescribe creams or medications to help you feel more relaxed.
Before your appointment
You may find it helpful to:
- plan your journey
- listen to music or watch something on your phone to help you relax, or bring something to read
- consider what to wear to your appointment; if you feel more comfortable wearing a skirt, dress or long top, it may help you feel more covered (you can keep these clothes on during your test and only take off your underwear)
- speak to the health professional beforehand to discuss your concerns if you think the test may be uncomfortable as they can offer support
- ask someone you trust to go with you, such as a friend, relative or carer/mental health worker, who can also be with you after your appointment
Questions to ask the health professional
It might be helpful to think of any questions you want to ask the health professional before your appointment.
We want to make you feel at ease so you have the best possible experience – you can ask for extra support for any reason, including if you:
- have a mental health condition
- take medication that makes you shake
- find it hard to leave your house
- sometimes find it hard to process information
- do not like to feel exposed by removing your clothes
- are embarrassed by showing your body
- have scars
- feel like you might be judged
- feel like a burden
- are afraid it will hurt
- may start to cry or freeze up
- may pass out or faint
- may have a panic attack
- get distressed during a physical examination
- have had a negative cervical screening experience in the past
- have experienced trauma
- are a survivor of sexual violence
- are a survivor of female genital mutilation or cutting (FGM/C)
- want to be warned before the health professional touches you
- find that waiting rooms make your symptoms worse
- find that certain words, actions or positions trigger anxiety attacks or flashbacks
You may want to print out and fill in the extra support checklist to take with you to your screening test.
During your appointment
The cervical screening test takes a few minutes – here’s what to expect at your appointment:
The health professional will explain the test at the start of your appointment.
- You will have a private space to undress from the waist down and you will have a modesty sheet to cover you – remember you can wear a long top or dress/skirt to help you feel less exposed.
- There may be different positions that could make the test more comfortable for you, like lying on your side. Your healthcare professional will work with you to make sure you are in the most comfortable position.
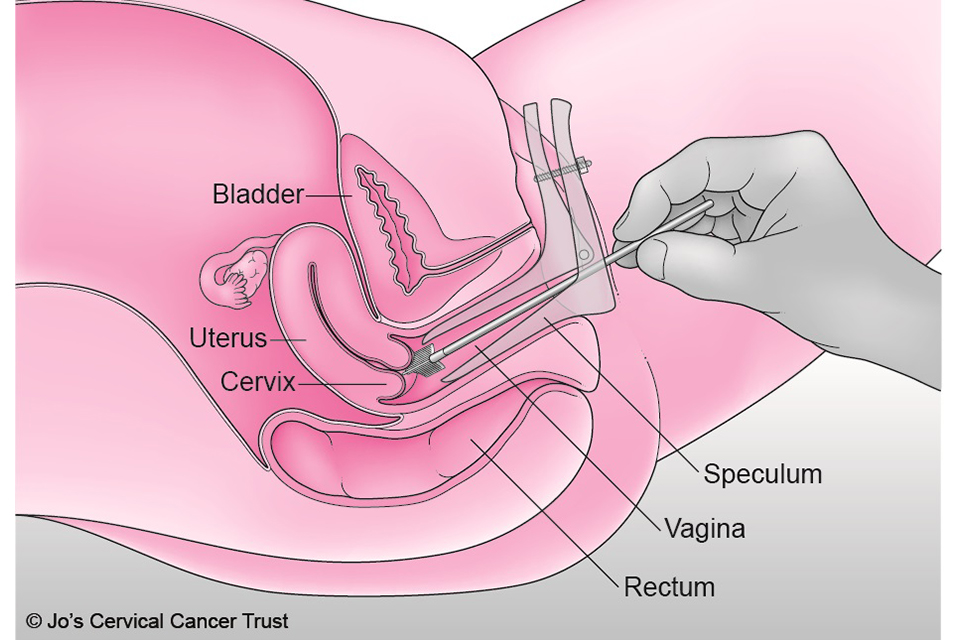
- A speculum (usually plastic) will be gently put into your vagina. It opens so the health professional can see your cervix. Speculums come in a range of sizes. Talk to your health professional to discuss the size that is most appropriate for you.
- The health professional will use a small, soft brush to take a sample of cells from your cervix.
- Your test could feel uncomfortable but remember, you are in control during the test. It may help to agree a word or hand signal, so the health professional knows to stop immediately if you want them to.
After the test
The sample of cells is sent to the laboratory for testing.
We will send your screening result to you by post. The nurse or doctor who does your screening test will tell you when you can expect to get your result letter, and they will also get a copy. Please make sure you tell your GP practice or healthcare professional about any changes to your address.
You may feel anxious while waiting for your results. It may help to speak with someone you trust about how you are feeling.
Cervical screening results
HPV negative
Most people get an HPV negative result. This means no further tests are needed and you will be called back for screening when your next test is due.
HPV positive, no abnormal cells
If your sample is HPV positive, we also test it for abnormal cells. If none are found, your result will say you have HPV, but no abnormal cells. We will ask you to come for screening again sooner than usual. Your result letter will explain when.
HPV positive, abnormal cells
There are several ‘grades’ of abnormal cells as some are more serious than others. Your result letter will explain what your results mean. If you have HPV and any grade of abnormal cervical cells we will refer you for colposcopy (see information below).
Further information about having a colposcopy is available at: NHS cervical screening – having a colposcopy.
Unavailable or inadequate
Occasionally a sample may be called ‘unavailable’ or ‘inadequate’. This means that we were not able to get a result from your screening sample. This sometimes happens when there are not enough cells in the sample to get a result or due to a technical problem at the laboratory.
We will send you a letter inviting you for a repeat test in 3 months. Waiting 3 months gives your body enough time to make new cells, meaning it is less likely to happen again.
Looking after your health
You will get another invitation through the post when you are due for cervical screening again.
If you have any unusual symptoms, please tell your GP as soon as possible. These might include:
- vaginal bleeding that is unusual for you; bleeding between your periods, during or after sex, after the menopause or having heavier periods than usual
- pain during sex
- changes to vaginal discharge
- pain in your lower back, between your hip bones (pelvis), or in your lower tummy (abdomen)
These symptoms are often caused by other things, but it is important to get them checked. In rare cases cervical cancer can develop in between screening tests. But if you are found to have cancer, getting it diagnosed and treated early can mean you are more likely to survive.
Screening is not a test for investigating symptoms. If you have any of these changes, don’t wait for your next cervical screening appointment. See your GP as soon as possible. Your GP can examine you and refer you to a gynaecology clinic if necessary.
Getting support
If you need support, you:
- can talk to a trusted friend, relative or health professional
- may find it helpful to seek spiritual support from a religious or spiritual leader
- may want to talk to someone at Jo’s Cervical Cancer Trust, The Havens, Samaritans or SANE
Jo’s Cervical Cancer Trust
Jo’s Cervical Cancer Trust is a national charity dedicated to eliminating cervical cancer that has information and support about cervical screening, cell changes (abnormal cells) and cervical cancer – no question too big or small.
More information about their Helpline (0808 802 8000) and online services can be found at Get Support – Jo’s Cervical Cancer Trust
The Havens
The Havens are specialist centres in London for people who have been raped or sexually abused. Telephone 020 3299 6900 for urgent advice or an appointment.
My Body Back (London and Glasgow)
My Body Back offers support to people to reclaim control of their body after sexual violence. It runs specialist clinics offering cervical screening and sexually transmitted infection (STI) testing in London and Glasgow for women, transgender and non-binary people who have experienced sexual violence.
Email: info@mybodybackproject.com
Samaritans
Samaritans is available round the clock, every single day of the year. You can talk to them any time you like, in your own way, about whatever’s getting to you.
Call free, any time: 116 123
Email: jo@samaritans.org
SANE
SANE is a national mental health helpline offering specialist emotional support to anyone affected by mental illness.
SANEline: 0300 304 7000 (every day, 4.30 to 10pm).
Support for victims of sexual violence and abuse
Advice and support for those who are experiencing or feel at risk of sexual violence and abuse is available at: Support for victims of sexual violence and abuse – GOV.UK (www.gov.uk)
National FGM Support Clinics
National FGM Support Clinics (NFGMSCs) are community-based clinics that offer a range of support services for women with female genital mutilation (FGM)
More information and clinic locations can be found at: National FGM Support Clinics – NHS – NHS (www.nhs.uk)
Acknowledgement
This information is adapted from a leaflet developed by Dr Frederique Lamontagne-Godwin, which was based on research with users of mental health services and was supported by:
- Jo’s Cervical Cancer Trust
- NHS Dorset Healthcare University Foundation Trust
- University of Surrey
- University of West London
- West London NHS Trust
We are grateful to all the patients, service user groups, professionals and frontline staff who helped in the making of that leaflet.
Transgender Patients
Information for Transgender Patients
Information for Trans Patients – Or those wishing to change their name, title and / or gender on their NHS records
We are proud to have you as our patient.
We support all patient groups and are committed to accessibility and inclusion, but we also know we may not always get things right. If there is anything you think we can improve or change to make accessing our services easier for you, please email bnssg.montpelierhealthcentre@nhs.net
Confidentiality
We hold your medical records in the strictest confidence, regardless of whether they are electronic or paper. We take all reasonable precautions to prevent unauthorised access to your records. Access to medical records is audited. Your NHS records are only shared with our Practice team and other organisations directly involved in your care that have a genuine need for it e.g. community health services, hospitals, mental health services, social care, NHS 111. We will not share your information with any other third party without your permission unless it is an exceptional situation (e.g. life or death situation) or where the law tells us to. For more information on how your data is shared and stored by the NHS, including opting out of sharing data, please see here
- Changing your name on your NHS records – Please fill out a change of name form available here or at reception. Please hand the form into reception or email to us bnssg.montpelierhealthcentre@nhs.net. No proof of ID is needed. This name will be used by staff, on the automated call-in screen, and communications from the Practice e.g. SMS, letters, email. You can request to change it at any time.
- Changing your title on your NHS records – you can change your title on your NHS records to any of Mr/Mx/Miss/Mrs/Ms without changing your gender or name. No proof of ID is needed. Just ask any member of staff or email us at bnssg.montpelierhealthcentre@nhs.net. The NHS computer system is currently binary and the only titles it currently accepts with a male gender marker are Mr or Mx. The only titles the computer system accepts with a female gender marker are Mx/Miss/Mrs/Ms. This computer system and titles available are set nationally and are out of our hand. If you wish to choose another title, we can add an alert to your notes, so we as a Practice know your gender identity, please discuss with any staff member
- Changing your gender marker on your NHS records to male or female– you can do this at any time, please book an appointment (ideally face to face) with a GP to discuss this. No proof of ID is needed. You do not need to have undergone any form of gender affirmation treatment, have been referred to a gender identity clinic or have any official documentation. Changing your gender will mean you will be allocated a new NHS number, and your pre-existing NHS number will no longer be accessible. Your previous notes will be merged to your new notes, minus any previous identity information. Any subsequent changes to gender would involve a further NHS number.
How long will the process take?
A new NHS number can take over 4 weeks to come through to us, once we notify PCSE . Once we receive your new NHS number, we will create a new registration for you at the practice within 5 days and will aim to merge your old records to your new records (excluding any information related to your previous identity) in a timely manner to ensure minimal disruption to your care. We suggest you order 2 months’ supply of your medication beforehand. You should be informed of your new NHS number by PCSE. If you do not receive this, please contact us and we can give it to you. You may need to inform any hospitals you are under (e.g., waiting for an appointment, surgery or treatment) of your new NHS number so they can update your records.
Cancer screening tests
Unfortunately, currently national cancer screening test invitations are sent out based on the gender marker on your NHS records. This system is currently very binary and only accepts a male or female gender marker on NHS medical notes. This is a national decision and out of our hands. If you wish to choose non-binary or another gender identity, we can add an alert to your notes, so we as a Practice know your gender identity, please discuss with a GP (see below).
Importantly patients who have changed their gender marker on their NHS records may not be invited to some of these cancer screenings, meaning there is a risk of missing cancer. Please see NHS screening Guidance for Trans Patients for more information. Please discuss with your named GP to make discuss this further.
Cervical cancer screening in trans men and non-binary people with a cervix
We welcome you to have your cervical screening at the GP surgery by highly trained staff. Please book a telephone appointment with a GP or nurse who performs cervical screening to discuss this.
Please see this NHS video on cervical screening in trans men here
We can also offer adaptions e.g.
- an appointment at the beginning or end of the clinic
- bring a friend/partner, bring your own blanket to cover the lower half of your body
- choose to have the door locked or unlocked
- chaperone in the room
- bring a phone/tablet and headphones to play music or watch a video
- different sizes of medical equipment – you can take one home with you to practice with beforehand if this is helpful
- At your appointment, other people in the waiting room will be waiting for a range of different appointments and will not be aware you are there for cervical screening
- Medication and lubricant to make the procedure more comfortable
You can also contact a specialist NHS clinic to have your cervical screening there (nearest is London):
- 56T at 56 Dean Street in London >
- The Butterfly Clinic in Liverpool >
- Clinic T in Brighton >
- CliniQ in London >
- My Body Back in London >
- My Body Back in Glasgow >
Discussion with named GP Once we receive your gender marker change form, we will book you a GP appointment to discuss cancer screening tests and merging your old and new notes.
Referral to an NHS Gender Identity Clinic Please book a GP appointment to discuss referral – you do not need to have socially transitioned, have counselling or psychotherapy or any tests for the referral. We will send the referral as soon as you request it. You can choose which GIC to be referred to see here. Hormone therapy can reduce your fertility, please let your GP know if would like to be referred to discuss egg or sperm storage whilst waiting for your appointment at the gender clinic. Your GP can also discuss other ways to support you whilst awaiting your appointment e.g., medications to stop periods and ensuring your physical health is optimised ready for hormone treatment.
Private Providers – Gender Identity Clinics
In the UK there are a number of private gender identity services, ranging from those mirroring the NHS offer – led by a team of clinicians (including doctors, psychologists) who also work at NHS gender clinics. Other clinics do not offer the equivalent of the NHS service e.g., online service only, do not have GMC registered doctors and are not UK based. We are unable to recommend any specific clinics. However, signs of a safe and effective service according to NHS England’s current commissioning protocol (2013) would be:
- The assessment and diagnosis of gender dysphoria is made by a clinician e.g., psychologist who specialises and is experienced in gender dysphoria. This is over a minimum of two core assessment consultations
- They ask for your full medical history
- The decision to start hormone therapy is made by a doctor who is registered and based in the UK, has relevant training in gender dysphoria and at least two years’ experience working in a specialised gender dysphoria practice, such as an NHS Gender Identity Clinic
- The clinic is based in the UK
- They discuss the following with you and give you opportunities to ask questions:
- potential risks and limitations of, and alternatives to hormone therapy, as well as its potential benefits
- The likely impact of hormone therapy on fertility including egg or sperm storage and how to access this.
- The likely permanent changes that hormone therapy will make to your body
- When on hormone therapy the need for effective contraception, regular monitoring (blood tests, blood pressure, weight), smoking cessation, maintaining a healthy weight. Also, what changes you should make to your medication if you were to have an operation
Local Support Groups
- TransBristol – a safe space where trans identified people in Bristol can share ideas, provide support and plan things.
- Bristol Crossroads – a safe, secure, friendly social meeting place for TG people of all kinds and those questioning their gender, their partners and close family. A community support group run by volunteers,
- Gay West website is a social and support group for LGBT people in Bath, Bristol, and surrounding areas.
- Hidayah website are a charity providing support, mentoring, and social connection opportunities to LGBTQI+ Muslims.
- LGBTQ+ support services for young people, their carers and families here
Montpelier Health discussion with GP about changing gender marker on NHS records
Please note, no proof of ID is necessary, you do not need to have undergone any form of gender affirmation treatment, have been referred to a gender identity clinic or have any official documentation.
Patient Name
Patient Address
Patient DOB
We support all patient groups and are committed to accessibility and inclusion but we also know we may not always get things right. If there is anything you think we can improve or change to make accessing our services easier for you, please let us know.
The aim of this document is to inform you of the process, discuss how your medical information is stored and the important screening tests you need. We hope that it is helpful.
The process of changing gender marker on your NHS records
When you change your gender marker on your NHS records, you will be given a new NHS number. Your previous NHS records will be merged onto your new NHS record (excluding any information related to my previous identity e.g., gender, title, name, pronouns, previous NHS number). This process is not reversible. Should you wish to revert back to your original gender marker, you would receive a third NHS number. This system is currently very binary and only accepts a male or female gender marker on your NHS records. This is a national process and out of our hands. If you wish to choose non-binary or another gender identity, we can add an alert to your notes, so we as a Practice know your gender identity.
A new NHS number can take over 4 weeks to come through to us. Once we receive your new NHS number, we will create a new registration for you at the practice within 5 days to ensure minimal interruption to your care. We will aim to merge your old records to your new records (excluding any information related to your previous identity) in a timely manner. You should be informed of your new NHS number by PCSE. If you do not receive this, please contact us and we can give it to you. Please also inform any hospitals you are currently under (e.g., outpatients, surgery waiting lists etc.) of your new NHS number so they can update your records.
Consider prescribing 2 months’ supply of current medication in advance of doing this process so that medication supply is not interrupted.
Dietician
This service is provided at a PCN level.
Dietitians work within primary care to assess, diagnose and treat dietary and nutritional problems at an individual and wider public health level. Dietitians use the most up-to-date public health and scientific research on food, health and disease which they translate into practical guidance. They utilise behaviour modification methods and motivational interviewing techniques as well as innovative digital practice to enable service users to make appropriate lifestyle and food choices to manage their own conditions, and so have a significant impact on clinical outcomes.
For more information about our Dietician, see the Meet the Team page.
Common Ambition
Improving HIV and sexual health services for people of African and Caribbean heritage in Bristol
Common Ambition Bristol (CAB) is a major 3- year community powered project led by Brigstowe working with the African and Caribbean heritage communities in Bristol to reduce HIV diagnosis, stigma and generally improve sexual health.
Common Ambition Bristol now has its own website! To find out more about this exciting project please visit CAB at www.commonambitionbristol.org.uk
You can also attend their monthly drop in service at MHC, each first Thursday of the month in the afternoon.

NHS Talking Therapy (Vitaminds)
If you are suffering from anxiety, depression, post-traumatic stress disorder, low mood or excessive worry, VitaMinds can provide you with advice, guidance and support.
Vita Health offer a range of short term psychological therapies to adults 16 years and over, who live and are registered with a GP in Bristol, North Somerset and South Gloucestershire. For more information, go to NHS Talking Therapy | Vita Health Group.

NHS Health Check
Carers and Young Carers Support
Are you a carer – adult or young person? Do you provide unpaid care for a family member or a friend who has a disability, illness or who needs another form of support to manage their life, who otherwise would find this hard to manage on their own?
If so, please tell our Health Navigators. They will be able to put you in touch with our Carers Lead/Young Carers Lead who will be able to offer you support in a variety of ways.
A carer is someone who provides support to family or friends who could not manage without this help. This could be caring for a relative, a partner or friend who is ill, frail, disabled or is affected by mental ill-health or substance misuse. It includes young people who may be caring at home.
We would like to encourage all carers to register with the GP surgery. Carers often neglect their own health as they are looking after someone else. By keeping a carer fit and well, we can support them to look after the cared for person in the best way and also look after their own physical and emotional wellbeing.
If you are a carer please contact the practice and ask to be put on the surgery carers register. You will be given a carers pack with information about support services and how the practice can help you. In most cases we can then:
- Offer a free flu vaccination
- arrange flexible appointment times to meet the carers needs
- share information about the person you care for to help in their caring role
- let you know about other organisations that can help
Bristol & South Gloucestershire Carers Support Centre
Contact Carers Line on: 0117965 2200
Please let your doctor or a member of the surgery team know that you care for someone.
Do you worry about what would happen to the person you look after if you became seriously ill, or had an accident?
- You can carry a Carers’ Emergency Card which identifies you as a carer and has a personal identification number.
- If you are taken seriously ill or have an accident, anybody who finds you can ring the phone number on the card and tell the emergency response team that the person you care for needs help.
- This service is free and operates 24 hours a day, 7 days a week.
Pick up a Carers Emergency Card Scheme leaflet from the surgery or visit:
Useful Contact Numbers
- Bristol City Council Health and Social Care;
Care Direct 0117 922 2700:
www.bristol.gov.uk ; provides information, advice, assessment and commissions and arranges care and support services - South Gloucestershire Health and Social Care
Adult Duty Team 01454 866807 - The Integrated Carers Team (Bristol): 0117 3521668. Provides carers simple assessments.
- Carers Support Centre; Carersline 0117 965 2200:
www.carerssupportcentre.org.uk ; provides information, advice and services focussed on supporting carers - Well Aware; 0808 808 5252
www.wellaware.org.uk ; offers a database of health, wellbeing and community resources - Age UK: Bristol: 0117 929 7537 www.ageuk.org.uk/bristol
South Glos: 01454 411 707 www.ageuk.org.uk/southgloucestershire
Provides day care services, information, advice and advocacy to ensure a smooth transition into care for older people. - Alzheimer’s Society: (Bristol and South Glos) 0117 9610 693
www.alzheimers.org.uk
Provides a range of services including dementia cafes, carers support groups, singing for the brain. - Health Links: (Bristol) 0117 902 7115 or 07900264435
www.briscomhealth.org.uk provide interpreters for health professionals - Carers Direct; 0808 8020202;
Website www.nhs.uk/CarersDirect ; provides a free national service offering information, advice and support for carers
ROADS (Recovery Orientated Alcohol and Drugs Service)
Bristol ROADS (Recovery Orientated Alcohol and Drugs Service) is a partnership between four core organisations:
- Developing Health and Independence (DHI)
- Bristol Drugs Project (BDP)
- Avon and Wiltshire Mental Health Partnership NHS Trust
- Addiction Recovery for All (ARA)
ROADS partners operate a ‘no wrong door’ approach which means even if your needs are best met by a different part of the system your referral will be transferred to the right part.
It also provides information/ advice on referrals for professionals, those who would like to access drug and alcohol support and families/carers of those who use drugs and alcohol.
Developing Health and Independence (DHI)
DHI is your first port of call for all referrals, except GP referrals.
The referrals include self and family or carer referrals, professional referrals from the NHS and Local Authority and from other agencies in Bristol.
For ROADS-wide general advice and support first visit Developing Health and Independence.
DHI will undertake a triage and then a full assessment within 7 days of your referral.
If your needs are better met with other agencies such as ARA, BDP or AWP they will arrange this for you and pass the required information across.
Service treatments and locations
DHI run several treatment and recovery services across its 3 hubs in the city:
- Bristol Central: Brunswick Court, Brunswick Square, St Pauls, Bristol, BS2 8PE
- South Bristol: Symes Community Centre, Peterson Avenue, Hartcliffe, BS13 0BE
- North Bristol: Greenway Centre, Doncaster Road, Southmead, Bristol, BS10 5PY
Services include:
- structured and unstructured 121 and groupwork (psycho-social interventions)
- a very well-developed Peer Support programme
- support services for carers
DHI also provide a self-help portal where you can find specific information on drugs and alcohol.
If you’re in the criminal justice system
DHI also run a service specifically for those in the criminal justice system, such as if you’re being released from prison, or have a probation officer.
This service is run from their premises at E5, Kings Square, 16-18 Kings Square, BS2 8AZ.
Family and carer support
DHI offers support to the families and/ or carers of those who use alcohol and other drugs.
These include:
- Help from other family members in similar situations
- Structured support groups
- Specialist support groups for the parents of teenagers using drugs or alcohol
- 1:1 session for support, advice, and counselling
- Reach Out, a dedicated annual conference for families and carers
For information on how to access DHI services, you can:
- call: 0117 440 0540
- email: roads@dhi-services.org.uk
- visit: DHI Families Also Matter
Bristol Drugs Project (BDP)
Bristol Drugs Project run the City’s GP-facing Substance Misuse Liaison and Rapid Access Alcohol Service.
GPs can refer all patients through the direct online booking system.
This can provide service users with a named worker and appointment time in their GP Practice or nearby which should take place within 7 days of referral.
If you’re a GP, access the Bristol Drug and Alcohol Service (Remedy BNSSG ICB) for clinical pathways and guidelines.
Walk in and outreach services
BDP provides a diverse range of early engagement outreach and groupwork and walk in services on weekdays and Saturday mornings at 11 Brunswick Square, St Paul’s, Bristol BS2 8PE.
These services include:
- Needle exchange, also through pharmacies
- Blood borne virus testing
- Naloxone and Nitazene Testing Strips
- Crack pipes
- Drug testing service, in partnership with the The Loop
- Community support services
BDP also run several specialist support services for different communities in Bristol:
- Wet Clinic: provides access to a GP for people who are alcohol dependent and struggle to access primary care.
- Women’s Morning: a weekly social support group for people who identify as female with a free creche service available.
- Prism: LGBTQ+: Bookable appointments with a specialist worker as well as access to clean injecting equipment and other harm reduction materials.
- The 50+ Crowd: A social support group for older people.
Recovery services
The service also offers a vibrant range of recovery community activities which are free to access.
Avon and Wiltshire Mental Health Services
Avon and Wiltshire Mental Health Services provide a range of specialised services.
These include:
- support for complex prescribing and detoxification
- an in-patient unit (ACER)
- a specialist psychology service
You cannot directly refer to these services.
Referral process
Once assessed and in ROADS under either BDP or DHI you may be referred to receive one of these services as part of your overall package of care if that is appropriate.
Referral process for professional carers
There is a referral process for professionals who care for patients who have difficulty controlling or eliminating their drug or alcohol use.
Contact our team at Acer Substance Misuse Recovery:
- Call: 0117 378 7980
- Email: awp.AcerUnitReferrals@nhs.net
The team will then give advice on making a referral.
Addiction Recovery for All (ARA)
Addiction Recovery for All promote tenancy sustainment and prevent homelessness for clients who use drug and alcohol.
They provide targeted interventions, promoting inclusivity and social integration, and meeting the needs of marginalised groups.
ARA have 2 relevant services:
- Homelessness Pathway 4
- Specialist Supported Housing
These support people with drug and alcohol needs who are at risk of losing their home.
Contact details for the public
For more information call 0117 930 0282
Professional referrals
If you are a professional, you can refer someone through the Housing Support Register.
Individual Placement and Support (IPS)
Individual Placement and Support offers intensive, personalised employment support to people accessing drug and alcohol services.
Contact IPS
Email: mariana.law@richmondfellowship.org.uk
Call: 01380 737 676
Professional referrals
Criminal Justice referrals
For all professional referrals involved in the Criminal Justice System who are living in Bristol with a Drug or Alcohol treatment need will be referred via the criminal justice single point of contact (SPOC).
This includes:
- Drug Rehabilitation Requirements (DRR’s)
- Alcohol Treatment Requirements (ATR’s)
To make a referral, or for more information and referral criteria
- Email: bristolcjit@dhi-online.org.uk.cjsm.net
- Call: 0122 598 3066
Mental health referrals
For Mental Health Treatment Requirements (MHTR) referrals contact:
Other professional referrals
All other professional referrers should:
- complete the docxROADS Referral Form (docx, 111 KB)
- email it to roads@dhi-services.org.uk
See the pdfROADS Delivery Model (pdf, 406 KB), an overview of substance misuse treatment provision in Bristol.
For young people
Bristol Drugs Project: Youth Team
The Youth Team at Bristol Drugs Project (BDP) supports young people who live in Bristol and who use alcohol or drugs.
They work with young people aged 11 to 19 years, or up to aged 24 if they have a learning difficulty or disability.
The team also offers support to young people who are concerned about a family member who uses drugs or alcohol.
They aim to help young people deal with problems early, before they experience a greater level of harm.
To make a referral, you can:
- Email: youthreferrals@bdp.org.uk
- Call: 0117 987 6008
- Visit: Make a referral to BDP Youth Team: Bristol Drugs Project
Young People’s Substance Misuse Treatment Service
The Young People’s Specialist Substance Misuse Treatment Service works with:
- young people under 18 who use any drug or alcohol
- who have additional mental health needs alongside their substance use
This service is part of the Children and Adolescent Mental Health Services (CAMHS).
To speak to a member of staff or to make a referral, call 0117 342 5729.
Drugs and Young People’s Project (DYPP)
The Drugs and Young People’s Project (DYPP) provides support for children and young people under 18 who:
- have a social worker
- use any drug or alcohol themselves
- or are affected by a parent or carer’s substance use
They also support some young people who work with Families in Focus.
DYPP Social work referrals
Referrals can be made by the social worker or Families in Focus worker, call 0117 377 2997.
Mutual aid
Self-help groups for people experiencing difficulties with drugs or alcohol:
National advice services
FRANK, the national drug and alcohol advisory service
